You can get in touch with me by telephone or text during normal business hours, through the email form below, or by postal mail at the address listed below.
For emergencies, please call, do not use the contact form.
Contact
Contact Information
484-447-6945
P.O. Box 5011
Limerick, PA 19464
drjessvet.com
Anaplasmosis
A Tick-Borne Disease on the Rise in Horses.
Posted on: January 19, 2014
Anaplasmosis
Also known as equine granulocytic ehrlichiosis, is a bacterial infection that is spread by deer ticks, the same tick that can spread Lyme's disease. Infected ticks can harbor either one or both organisms at the same time and infect a horse with Lyme's and anaplasmosis with one bite. Infection with Anaplasma phagocytophilum targets a certain type of white blood cells, and signs can be seen up to 3 weeks post-inoculation. I usually see more cases of anaplasmosis starting in the late fall after tick season, and continuing into the spring.
Many of the horses that end up being diagnosed with this disease initially fall into the diagnostic category we veterinarians like to call “ADR”, for “Aint doin' right”. They may seem chronically depressed or slower than normal, slightly achy, or have just been losing weight slowly despite the owner's best attempts to maintain it. More acute cases show more obvious outward signs such as fever, swelling in one or multiple legs, ventral edema (swelling along the underside of the belly), pinpoint hemorrhages on the gums called “petechiae”, icterus (yellowing of mucous membranes such as the gums or whites of the eyes), neck pain, and reluctance to move. A horse can show any combination of these signs, and the signs themselves are not specific to infection with anaplasmosis.
 We can verify our hunch that a horse is infected with blood tests. I carry a quick test kit on my truck called a SNAP or Lyme 4Dx, that was designed to test dogs for Lyme's, anaplasmosis, heartworm and ehrlichiosis, but works very well to detect Lyme's and anaplasmosis in horses too. Three drops of blood and about ten minutes is all I need to do a good screening test for the two most common tick-borne diseases in the area. Sometimes we can see the organisms inside the white blood cells they attack under the microscope on blood sample smears. Blood can also be sent to an outside laboratory to determine an actual titer to the organism. CBC tests on horses with anaplasmosis often show anemia and thrombocytopenia (low platelet count), which explains why some horses with severe or more chronic infections may have problems with bleeding and clotting.
We can verify our hunch that a horse is infected with blood tests. I carry a quick test kit on my truck called a SNAP or Lyme 4Dx, that was designed to test dogs for Lyme's, anaplasmosis, heartworm and ehrlichiosis, but works very well to detect Lyme's and anaplasmosis in horses too. Three drops of blood and about ten minutes is all I need to do a good screening test for the two most common tick-borne diseases in the area. Sometimes we can see the organisms inside the white blood cells they attack under the microscope on blood sample smears. Blood can also be sent to an outside laboratory to determine an actual titer to the organism. CBC tests on horses with anaplasmosis often show anemia and thrombocytopenia (low platelet count), which explains why some horses with severe or more chronic infections may have problems with bleeding and clotting.
Treatment for anaplasmosis consists of IV administration of the antibiotic oxytetracycline either once or twice a day for 7 days. Oxytetracycline is very irritating outside of the vein, so most horses will need to be seen daily by their veterinarian for treatment unless the client is skilled at IV injections or can maintain an IV catheter at home. Horses with swelling or a fever may also need anti-inflammatory drugs such as Banamine. Usually we see some improvement in signs within about 3 days of starting treatment. Most horses recover easily, although those with complications or prolonged disease may have a poorer prognosis.
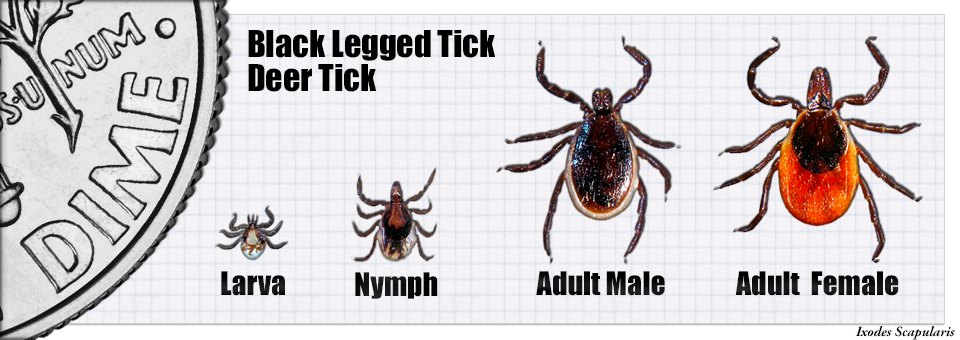
So what can you do to decrease your horse's chance of becoming infected? The most important thing to do is try to reduce your horse's exposure to ticks. Not all ticks are infected, but often the ones that pass on the disease are so young and small that they are difficult to see and remove. Regular grooming, especially after trail riding through brush or tall grass, can help detect ticks. Horses are able to groom themselves to some degree, but ticks tend to attach in areas where the horse cannot easily remove them, such as between the jaw bones and between the front and hind legs, and these are the places to check first. Keeping brush cleared from grazing areas will also help to reduce the tick habitat on the farm. Unfortunately there is no anaplasmosis vaccination available for horses.